News
Managing Movement Disorders
Sensorimotor lab looks for ways to improve patient care
On the fourth floor of Cooke Hall, high above the bustle and noise of offices and classrooms, there is a light-filled, spacious laboratory, immaculate and efficient. Here a group of talented and dedicated researchers and students are discovering ways to help people, many with debilitating movement challenges, enjoy a quality of life they never could have imagined.
The Human Sensorimotor Control Laboratory (HSCL), directed by School of Kinesiology Professor Jürgen Konczak, explores how the human brain controls movement. More specifically, the lab’s research focuses on how disease alters brain function that leads to movement disorders. Taking that mission a step further, the lab is committed to developing ways to help people with movement disorders manage their disability and live as fulfilling and independent lives as possible.
“A primary goal of the lab’s research is to enhance our understanding of the underlying mechanisms behind specific motor deficits, with the ultimate aim of translating such knowledge into new therapeutic approaches,” says Konczak. His team of graduate students, postdoctoral researchers, and research partners and collaborators from around the world, have researched, created, and tested devices and rehabilitation options to help treat some of the most challenging medical conditions, such as Parkinson’s disease, voice disorders, and stroke.
The laboratory also has a number of industry partnerships, providing expertise in human ergonomics, movement physiology, and biomechanics. HSCL has conducted human testing for federally funded and industry-sponsored studies that develop new health and safety products and has undertaken selected research for possible commercial applications. Examples include studying how the vibration behavior of a tennis racket design may mitigate muscle fatigue, and evaluating a new fastening mechanism design for a child’s car seat.
Over the past few years, the lab has consistently attracted external funding from agencies such as the German Science Foundation, the U.S. National Science Foundation, and the National Institutes of Health, as well as support through U of M grant programs from the Clinical and Translational Science Institute, the Office of Development and Translation, and the Jump Start program in CEHD.
Engaging in research to help people with physiological speech disorders
One of HSCL’s current research efforts centers on focal dystonia, a disease that affects a muscle or group of muscles in a specific part of the body, causing involuntary muscular contractions and abnormal postures. For example, a person’s neck muscles may contract unintentionally, resulting in abnormal and often painful head postures. Or, the muscles of the larynx controlling speech contract excessively, causing a permanently hoarse voice that makes it very difficult and exhaustive to communicate.
Spasmodic dysphonia (SD) is a type of focal dystonia that causes interruptions of speech and affects voice quality. The muscles inside the vocal folds experience sudden involuntary spasms, which interfere with the ability of the folds to vibrate and produce voice. People with SD may have occasional breaks in their voice every few sentences, or more often, may have spasms that occur every other word, making their speech difficult to understand. A patient describes living with this disorder: “My life is divided into two parts. Everything before SD, and everything after SD. Absolutely life-changing.” Another says, “SD has robbed me of my personality and kept me from living my life fully. I was a people person and loved to talk to everyone. Not anymore.”
Treatments for spasmodic dysphonia
Traditional treatment options for SD are limited. Injection of botulinum toxin into the laryngeal muscles controlling speech will partially paralyze the muscles, which can ameliorate voice symptoms for several months. However, only a subset of patients receive lasting benefits from this treatment. Deep brain stimulation has recently been promoted as another alternative, although this treatment requires brain surgery and there is little evidence of its effectiveness for treating SD symptoms. But recently, HSCL researchers made a remarkable discovery: in a preliminary study, vibro-tactile stimulation (VTS) of the larynx resulted in measurable improvements in the voice quality of people with SD.
Vibro-tactile stimulation
“We have been studying laryngeal dystonia since 2012,” says Konczak. “We discovered that people with this voice disorder have an underlying somatosensory deficit, which means their brain does not properly process signals that come from the receptors in the muscles. This gave us the idea to investigate if one can modulate the activity of this neural circuitry by applying vibration to the skin above the larynx with the goal to improve the voice symptoms of people with SD.”
Konczak says there is evidence that suggests that laryngeal VTS “normalizes” the way the brain processes signals from the muscles and then communicates with those muscles that are activated during speech, relieving symptoms in some patients. The results from preliminary studies with SD patients, which consisted of a one-time, 30-minute application of VTS, have encouraged HSCL researchers to explore VTS as a possible treatment for SD and other forms of dystonia. The National Institutes of Health recently awarded the HSCL $775,000 to conduct a systematic clinical trial to investigate possible longer-term benefits of VTS for people with SD. The NIH study involves participants with SD who will self-administer VTS at home for up to eight weeks.
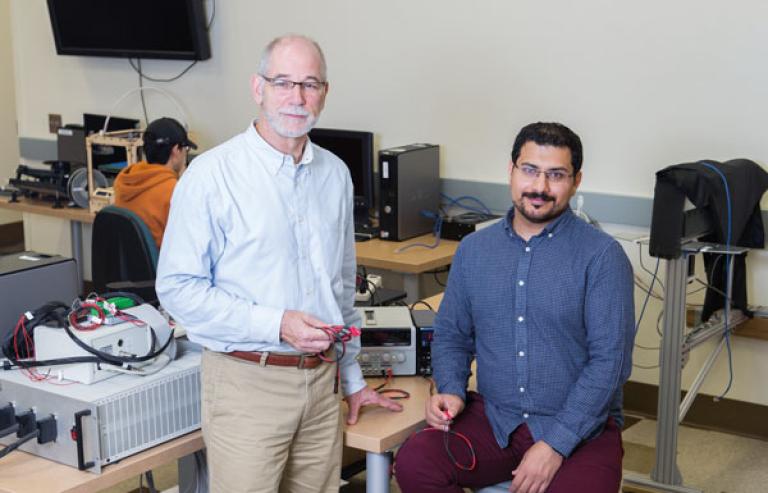
SD Voice Collar
Konczak and his team knew they needed to translate their neurophysiological findings into a therapeutic tool that could be easily used by people with SD. Biomedical engineers in the lab designed and prototyped a collar-like, wearable device that fits around the neck, can apply VTS, and is transportable. Their work on the SD Voice Collar has received funding from the University’s Clinical and Translational Science Institute to create a next-generation prototype that eventually can be manufactured and made available to patients with SD. Arash Mahnan, a biomedical engineer and doctoral student in HSCL, successfully created the first prototype.
Last June, the lab was awarded a $50,000 grant from the National Science Foundation (NSF) to conduct further study of the SD Voice Collar. The grant will support nationwide interviews with SD patients, otolaryngologists, speech therapists, and others in the medical device industry to determine the potential for making the SD Voice Collar available commercially.
“Our study findings will inform patients and clinicians on the possible impact of this therapeutic approach,” says Konczak, “and could promote the development of wearable VTS devices that would greatly expand the available therapeutic arsenal for treating voice symptoms in SD.”
The NSF study was completed in the fall of 2019. Its results will inform the HSCL researchers on the next steps in their development of the SD Voice Collar and on how the device can be brought to market and made available to patients.
Help for those recovering from the effects of stroke or who live with Parkinson’s disease
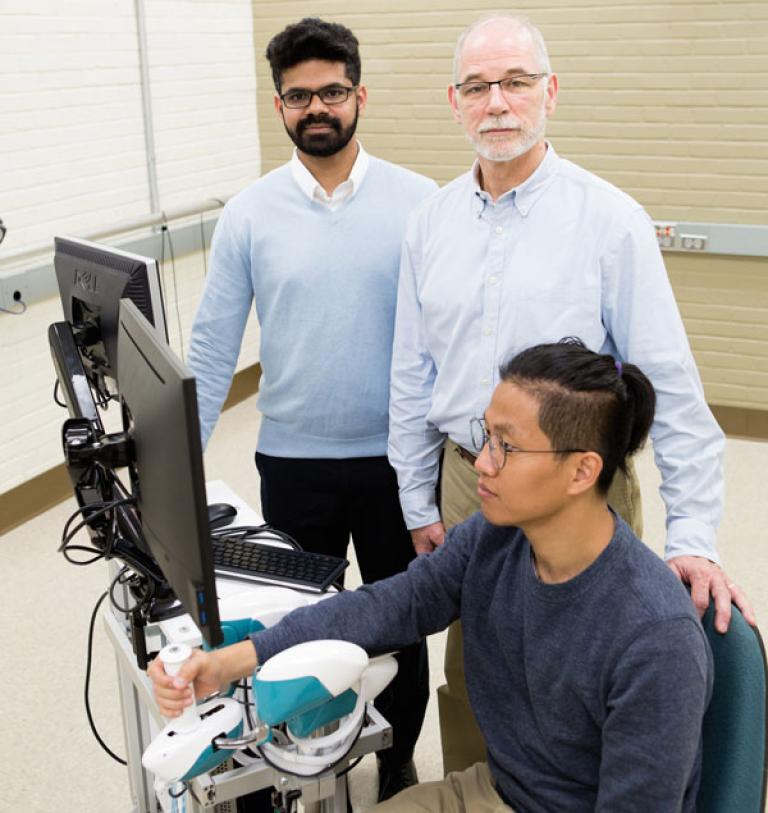
Another HSCL research initiative involves the development of robotic rehabilitation to help patients who are recovering from stroke or spinal cord injury. Many patients experience reduced body perception, or proprioception—the ability to sense or feel the limbs and body movements without seeing them. Often they lose motor function and experience somatosensory deficits, or the inability to interpret bodily sensation. This often occurs in the wrist, and can be a serious detriment to daily function and self-care.
Enter the WristBot, a robotic exoskeleton developed to assess and train proprioceptive and motor function of the hand and wrist. The glove-like device fits over the hand and leads patients through a series of exercises, designed as a game, to help them regain their wrist and hand movement.
“We’ve been collaborating with colleagues at the Italian Institute of Technology in Genova and Nanyang Technological University in Singapore over the past few years to develop this rehabilitation device,” says Konczak. The WristBot will likely find use in rehabilitation hospitals, he says, where most stroke patients spend their first days of recovery. “Moving the body as early and intensely as possible is beneficial to recovery, and the WristBot may induce a higher intensity of exercise than traditional physical therapy,” he says. The Wristbot’s gamified exercise also may motivate patients to practice longer and more vigorously.

HSCL is currently performing two clinical studies with stroke patients and patients with Parkinson’s disease to establish the efficacy of the WristBot. Dr. Naveen Elangovan, a certified physical therapist and postdoctoral researcher in the lab, is the lead investigator in this project.
“With the recent advances in robotics, it is possible to deliver highly engaging, customizable, and patient-centered robotic therapy for improving somatosensory and motor function in people with neurological impairments,” Elangovan says. “However, the available knowledge on the specifics of robotic sensorimotor rehabilitation is limited. The clinical studies from the lab will provide new critical insights on the application of robotics in the field of neurorehabilitation.”
Koczak sums up HSCL’s success—and commitment—to pioneering research initiatives that will improve lives this way: “Our lab engages in translational medicine,” he says. “We’re bridging basic and applied science in ways that will help us use our research findings to develop new therapies and medical applications. We need to understand disease mechanisms and we need to know basic science—without this we can’t make informed decisions about best therapies. We need both types of science.”
Story by Marta Fahrenz | Photos by Erica Loeks | Winter 2020
Read more about the Human Sensorimotor Control Laboratory.